How to improve the diagnosis of prostate cancer
Finding a new way to diagnose prostate cancer is on the minds of many urologists—and with good reason. Screening currently relies on a blood test looking for prostate-specific antigen (PSA), but there are serious doubts about the test’s accuracy.
A 2018 systematic review and meta-analysis examined data from more than 700,000 men in 5 separate studies, attempting to assess the impact of early detection of prostate cancer using a PSA test1. It found a large number of false-negative results: About 15% of men who had a negative PSA test developed prostate cancer within 7 years. Prostate tumors are usually slow-growing, which likely means that many cancers go undetected by the PSA test, thereby missing an opportunity to treat the disease early.
Part of Nature Outlook: Prostate Cancer
The review found even higher false-positive rates: about two-thirds of men who initially tested positive for PSA had a negative tissue biopsy. Other studies have shown similar error rates. This is one of the biggest concerns about the current screening system.
Prostate biopsies are the natural next step after a positive PSA test, but they are invasive and can cause a variety of complications. “We typically take 32 tissue cores for a biopsy,” explains Nathan Lawrenchuk, urological surgeon and oncologist at the Royal Melbourne Hospital in Australia. “That means you stick a needle in 32 times and each core has one to two centimeters of tissue. You can imagine that this is not pleasant.”
There are two main thoughts on how to replace PSA screening. The first is to look for better biomarkers in blood or urine, and the second is to forego examining samples altogether in favor of sophisticated imaging techniques. Whichever approach prevails, better screening with fewer false positives should mean fewer patients undergoing unnecessary biopsies.
Researchers say testing should also attempt to stratify risk. “They want to catch the aggressive cases, but there’s no good way to do that,” says Kevin Koo, head of assay development at diagnostics biotechnology company Xing Technologies in Brisbane, Australia. Many prostate cancers could certainly be left alone, but with a confirmed diagnosis comes the temptation to treat it — and like a biopsy, these treatments shouldn’t be taken lightly. Studies have shown that 17% of men undergoing surgery for prostate cancer suffer from urinary incontinence and 83% suffer from erectile dysfunction1. For those irradiated, it is 4% and 73% respectively1.
“The specificity of PSA is shocking,” says Koo. “You cast a big net and hope for the best.” A better biomarker that could both accurately confirm a diagnosis of prostate cancer and tell doctors about the risk of progression could help prevent overtreatment and improve people’s quality of life to obtain.
Biomarker hunt
As scientists research alternatives to PPE, they are keen to make sure they don’t lose one of PPE’s few advantages: its simplicity. No one wants to replace a non-invasive blood test with something that is more inconvenient for patients, more difficult to perform, or more likely to cause side effects. Therefore, most of these efforts are focused on finding biomarkers in blood or urine samples.
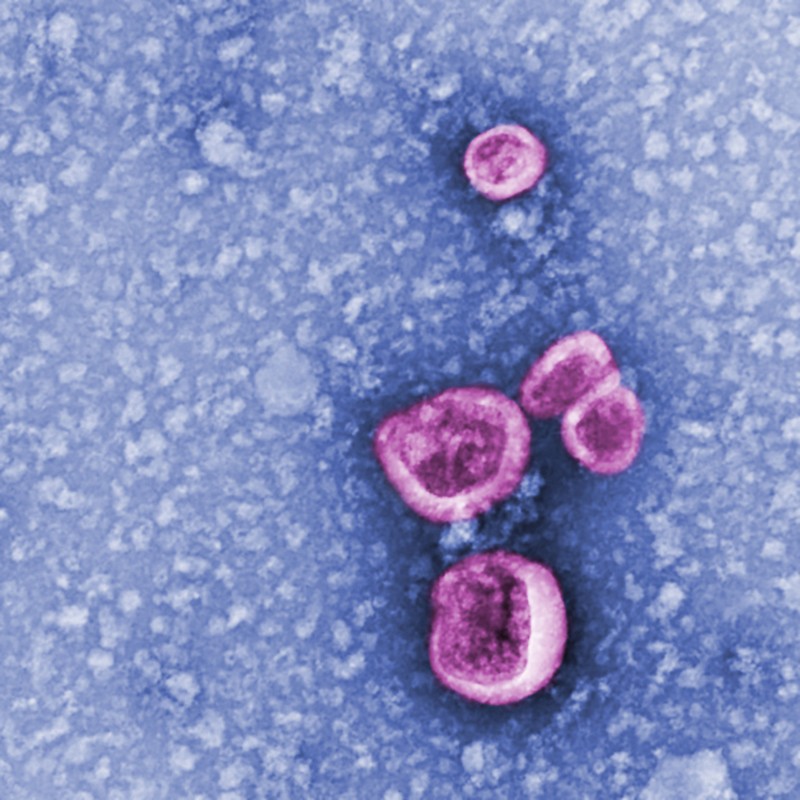
Exosomes are one such candidate. These nano-sized capsules are secreted by almost all cell types in the body and migrate to the extracellular matrix. Their cargo is often different from the cell they come from, meaning exosomes produced by prostate cancer cells could be easily identified.
When exosomes were discovered in the 1980s, scientists were unsure what to do with them. “At first they were thought to be basically garbage excretions, but we now know that exosomes can be a tool for cell-to-cell communication,” says Ayuko Hoshino, a molecular biologist at the Tokyo Institute of Technology who studies how exosomes spread can affect a cancer.
Cells produce and export exosomes for a variety of reasons, including in response to inflammation – they allow immune cells to talk to each other and coordinate their defenses against infection. Long-term inflammation can contribute to the development of prostate cancer, further underscoring the suitability of exosomes as a potential biomarker.
A study from 20192 characterized the exosomes of eight black men and eight white men with prostate cancer, as well as those of a matched control group composed of healthy participants with a similar racial balance. The researchers isolated exosomes from blood samples, quantified them and analyzed the proteins they contained.
Exosome concentrations in samples from people with prostate cancer were about 3.5 times higher than those without cancer. However, some of their content differed between black and white men. The researchers found 7 proteins that were found exclusively in the exosomes of black men with prostate cancer and 33 that were found only in the exosomes of white men with the disease.
Despite its small size, this study demonstrates the importance of considering different ethnic groups in the search for new avenues for prostate cancer screening. The current PSA test isn’t particularly accurate for any ethnicity, but it’s particularly problematic for black men because they typically produce significantly lower levels of PSA and are therefore less likely to reach the concern threshold. Black men are also at higher risk of developing prostate cancer and are more than twice as likely to die from the disease than white men.
Exosomes show promise as biomarkers, but scientists are also studying microRNA (miRNA). These are small, single-stranded, non-coding genetic sequences that float freely in body fluids.
A 2020 study identified distinct miRNA signatures in the blood of people with benign, localized, and advanced prostate cancer3. By examining the levels of four different miRNAs, the scientists were able to predict the outcome of biopsies more accurately than with PSA.
Others are researching miRNAs found in the urinary system. In another study from 20204, researchers analyzed the urine sediments of 50 men scheduled to undergo prostate biopsy, 26 of whom later had a positive result. The scientists looked for 12 different miRNAs previously associated with prostate cancer. Levels of two of these resulted in more accurate predictions than using the current PSA test.
Studies like these have garnered buzz that new blood and urine tests will eventually solve the PSA problem. But molecular biomarkers like exosomes and miRNAs aren’t the only game in town.
Imaging alternative
“People think we absolutely need biomarkers from blood or urine to solve the PSA problem,” says Lavrenchuk. “But before you get a prostate biopsy in Australia, you get an MRI [magnetic resonance imaging] scan, and most people will have something show up in the images before they get a biopsy.”
Advances in imaging technology mean that scans can now provide valuable information beyond just locating a prostate tumor. They can also help determine the severity of a tumor by showing if it has started to spread. For example, a 2019 review of 98 studies found that imaging tests such as transrectal ultrasonography, computed tomography, and MRI can detect prostate cancer even with low PSA levels5.
Machine learning — the use of computers and algorithms that can accurately extract information from large data sets without explicit instructions — looks particularly promising. Studies have already shown how the technology could be applied to medical imaging, performing image analysis and combining data from different scanning modalities to accurately identify potential cases of prostate cancer.
More from Nature Outlooks
“I think the advances in imaging are currently beating the biomarkers,” says Lavrenchuk. But it’s not really a question of one or the other – it could well be a combination of imaging and molecular biomarkers that will finally replace PSA.
However, many more studies are needed to convince regulators and insurance companies before a new diagnostic marker is introduced, says Paul Mainwaring, co-founder of Xing Technologies. “Delivering health system change is a slow and challenging process at many levels.”
This feeling is shared by Hoshino. The basic science underlying exosome-based diagnostics is solid, she says, but testing methods need to be refined to ensure they truly offer a better deal than PSA. “We need to do thorough testing to look for the best panel of exosome biomarkers that will give us a high level of sensitivity and specificity,” she says. The same is true for the other techniques under development – a critical mass of data is now needed to give scientists and physicians confidence that they are improving PSA levels.
Until such evidence is available, it is likely that any new test will complement, not replace, PSA. No doctor wants to misdiagnose a patient because they failed to perform a conventional test.
But Mainwaring is confident the field will get there. “We’re finally starting to see research funded on this question,” he says. Promising alternatives to PPE could do so much to prevent misdiagnosis and are taking shape.