Researchers Discover How to Overcome Treatment Resistance in HER2 Positive Breast Cancer
Researchers at the Hospital del Mar Medical Research Institute (IMIM) in Barcelona, Spain, have discovered how a treatment-resistance mechanism in one of the most aggressive types of breast cancer can be overcome by activating the body’s immune response.
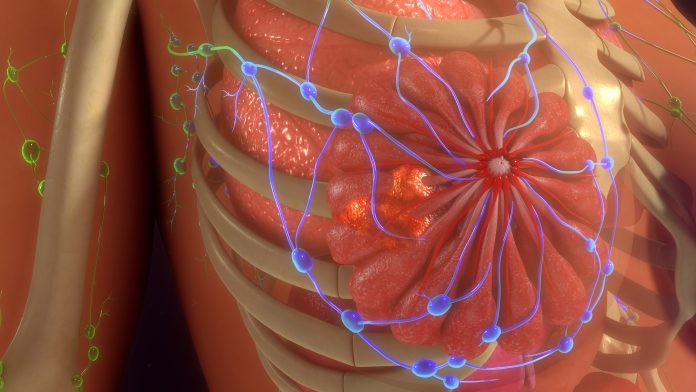
HER2-positive breast cancer tends to grow faster, spread, and come back more often than other types of the disease. In addition, tumors are surrounded by a microenvironment that protects them and allows them to develop resistance to antibody treatments such as trastuzumab, which normally allow immune cells to eliminate the cancer. Cells called fibroblasts play a key role in this process by blocking the immune system from trying to attack the tumor. A research team at IMIM is now trying to use these cells in a targeted manner to overcome resistance.
reporting nature communicationthe scientists identified a specific type of fibroblast called TGF-beta-activated fibroblasts that express a molecule called FAP that protects the tumor from immune cells. Using an ex vivo model with cells from breast cancer patients and trastuzumab as treatment, the researchers targeted FAP molecules with another molecule called FAP-IL2v and showed that resistance to the immune cells can be reversed.
“When this molecule, FAP-IL2v, is placed in contact with immune cells in an ex vivo replicated tumor containing this treatment-resistant microenvironment, the efficacy of trastuzumab is restored,” said Alexandre Calon, PhD, head of the Translational Tumor Research Microenvironment Laboratory at IMIM and Senior author of the study in a press statement.
Researchers validated the results with three cohorts of patients using over 120 samples. According to the study, in all samples, the number of activated fibroblasts directly affected the ability of the immune system to attack the tumor. The higher the fibroblast level, the more difficult it was for immune cells to target the cancer cells, despite antibody treatments like trastuzumab that activate the immune system.
Lead author Calon explained that this allows for better selection of patients who would benefit from FAP-IL2v treatment aimed at disabling the tumor microenvironment. “By filtering people based on these characteristics, we can isolate a population of treatment-resistant patients who can be targeted with this molecule to restore efficacy to breast cancer therapy,” Calon explained.
Other approaches exist for modifying the tumor microenvironment to improve drug delivery efficiency. A previous review article published in trends in cancer discusses the possibilities of redesigning the physical microenvironment of the tumor, such as B. Targeting the blood vessels surrounding a tumor in an attempt to deprive cancer cells of oxygen and nutrients in order to effectively eliminate them.
In conclusion, IMIM study co-author Joan Albanell, PhD, head of IMIM’s oncology department, said in a press statement: “The study identifies tumors in which resistance to anti-HER2 therapy is primarily mediated by one fibroblast type and not by another caused is caused. This important discovery should be used to design clinical trials of drugs that will overcome this resistance only for those patients in whom this resistance is effective. Here we need to move towards precision oncology.”